Case scenario
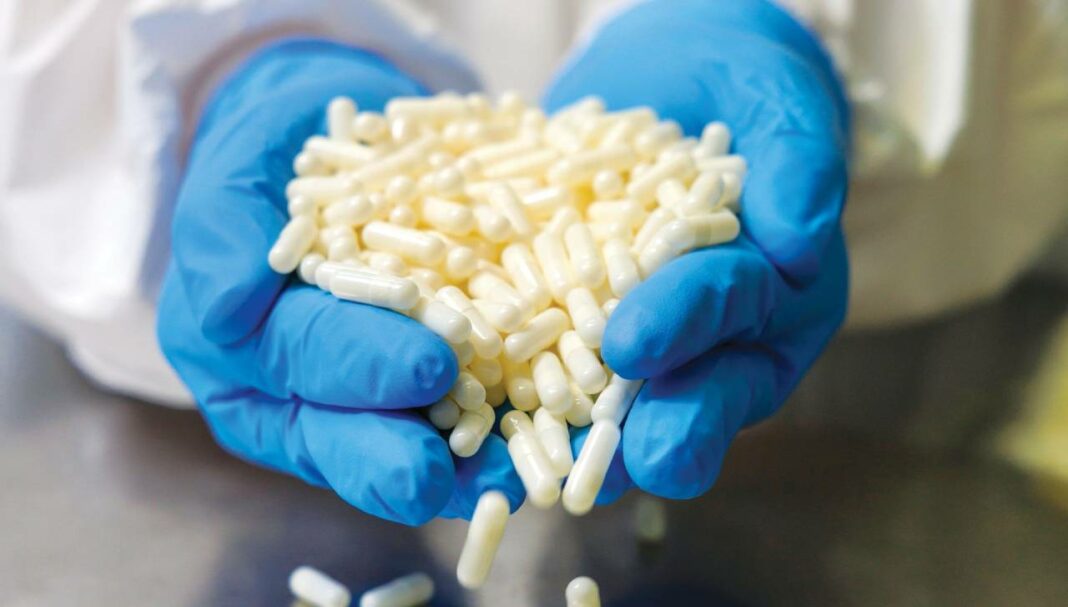
You are working in a compounding pharmacy and are presented with a prescription for an oral tacrolimus suspension for Patrick, aged 8, who has had an organ transplant. Due to the hazardous nature of tacrolimus, compounding the medicine requires
strict adherence to safety guidelines. You begin by reviewing the prescription and consulting the stability data and available formulations for compounded oral tacrolimus suspension. You gather the necessary ingredients and equipment required.
Learning objectivesAfter reading this article, pharmacists should be able to:
Competency standards (2016) addressed: 1.1, 1.3, 1.4, 1.5, 1.6, 3.4, 4.5 Accreditation number: CAP2406AMDS Accreditation expiry: 31/05/2027 |
Already read the CPD in the journal? Scroll to the bottom to SUBMIT ANSWERS.
Introduction
Hazardous medicines play an important role in modern healthcare, offering treatment for diverse diseases and conditions, such as cancer or the prevention of transplant rejection. However, their handling and compounding pose substantial risks to healthcar
THIS IS A CPD ARTICLE. YOU NEED TO BE A PSA MEMBER AND LOGGED IN TO READ MORE.